What is lipoprotein lpa cholesterol – What is lipoprotein (a) cholesterol? It’s a type of fat in your blood, and understanding it is crucial for cardiovascular health. This comprehensive guide delves into the specifics of lipoprotein (a), exploring its structure, function, link to heart disease, and available management strategies. We’ll also look at how genetics and lifestyle factors play a role in lipoprotein (a) levels.
Lipoprotein (a), often abbreviated as Lp(a), is a complex particle in the blood. It’s similar to LDL cholesterol, often called “bad” cholesterol, but with an added protein component that makes it particularly sticky and prone to contributing to plaque buildup in arteries. This buildup can lead to various cardiovascular issues, so knowing your Lp(a) levels is important.
Introduction to Lipoprotein(a)
Lipoprotein(a), often abbreviated as Lp(a), is a unique type of lipoprotein, a complex particle that transports cholesterol and other lipids throughout the body. Understanding Lp(a) is crucial because elevated levels are a significant risk factor for cardiovascular disease. This is a complex molecule, and its role in health and disease is still being fully elucidated.Lp(a) is distinct from other lipoproteins like LDL and HDL, exhibiting a complex structure and function that sets it apart.
Its presence in the body is associated with a higher chance of developing heart disease and stroke. This article will delve into the specifics of Lp(a), exploring its structure, function, and place within the broader context of lipid transport.
Structure and Composition of Lp(a)
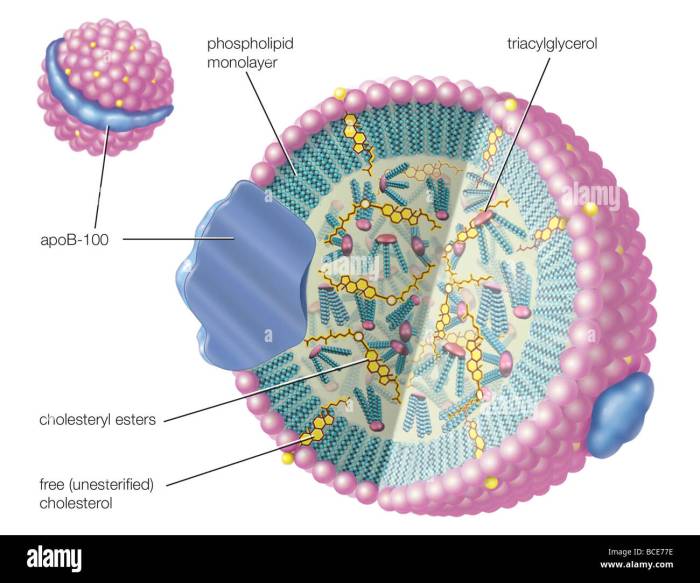
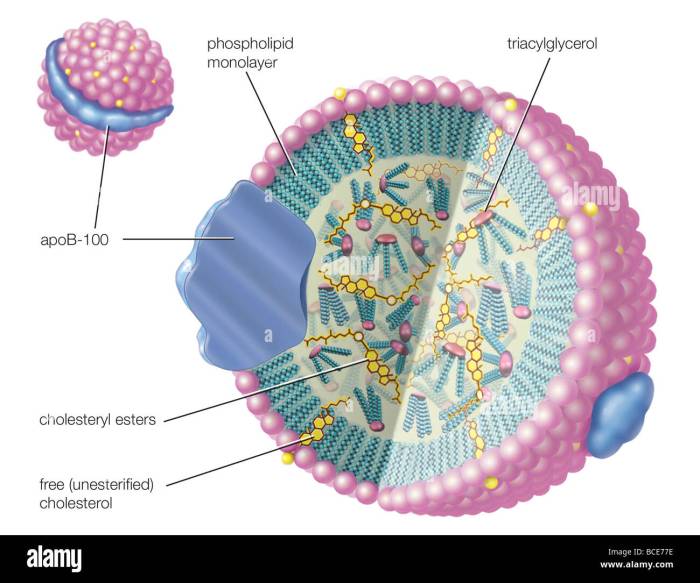
Lp(a) shares a fundamental structural similarity with low-density lipoprotein (LDL), but it also contains a unique component. Crucially, Lp(a) has an apolipoprotein(a) (apo(a)) molecule attached to an LDL core. This apo(a) component is a glycoprotein with a variable number of kringle IV-type repeats, which are protein structures. The length of this apo(a) component directly influences the Lp(a) particle’s size and potential impact on cardiovascular health.
Key Components Distinguishing Lp(a)
The defining feature of Lp(a) is the presence of apolipoprotein(a). This protein is structurally related to plasminogen, an enzyme involved in blood clot breakdown. The variable number of kringle IV repeats in apo(a) significantly affects the Lp(a) particle’s size and its interaction with the body’s systems. This unique structure gives Lp(a) its distinct properties, setting it apart from other lipoproteins.
Lipoprotein (a), or Lp(a), cholesterol is a type of cholesterol that’s often linked to heart disease risk. Figuring out your Lp(a) levels is a crucial part of your health journey, and understanding your options for managing it is important. Fortunately, navigating the world of career advice can be just as crucial as managing your cholesterol levels, especially right after graduation.
For a comprehensive guide on how to make the most of your next steps, check out this valuable resource on career advice college graduates. Ultimately, understanding your health, both physically and professionally, is key to a well-rounded life, and knowing your Lp(a) levels can help you take control of your health journey.
General Function of Lp(a)
Lp(a) plays a role in cholesterol transport, similar to LDL. However, its presence is also linked to inflammatory processes. The specific function of Lp(a) is not fully understood, but its association with atherosclerosis, a hardening and narrowing of the arteries, is well-documented. It’s suspected that Lp(a) may contribute to plaque buildup by inhibiting the body’s natural processes that break down clots.
Comparison of Lipoproteins
| Lipoprotein | Structure | Function |
|---|---|---|
| Lp(a) | A modified LDL particle with an apolipoprotein(a) (apo(a)) molecule attached. The length of the apo(a) molecule, characterized by varying numbers of kringle IV repeats, significantly impacts the particle’s size and properties. | Transports cholesterol, but also implicated in inflammatory processes and potential inhibition of clot breakdown. |
| LDL | A spherical particle primarily composed of cholesterol esters and apolipoprotein B-100. | Transports cholesterol from the liver to peripheral tissues. |
| HDL | Smaller, denser particle primarily composed of protein and a smaller amount of cholesterol. | Transports cholesterol from peripheral tissues back to the liver, often referred to as “good” cholesterol. |
Lp(a) and Cardiovascular Disease: What Is Lipoprotein Lpa Cholesterol
Lipoprotein(a), or Lp(a), is a unique type of lipoprotein that’s been linked to an increased risk of cardiovascular diseases. While the exact mechanisms are still being investigated, the presence of elevated Lp(a) levels is a significant factor in the development and progression of atherosclerosis. Understanding this connection is crucial for risk assessment and preventative strategies.Elevated Lp(a) levels are associated with a heightened risk of cardiovascular events.
This association stems from the complex interplay between Lp(a) and the processes that lead to atherosclerosis.
The Link Between Elevated Lp(a) and Cardiovascular Risk
Lp(a) shares structural similarities with LDL (“bad”) cholesterol, a well-established risk factor for heart disease. This shared structure allows Lp(a) to potentially contribute to the build-up of plaque in the arteries. The presence of Lp(a) can interfere with the body’s natural mechanisms for clearing cholesterol, potentially accelerating the development of atherosclerosis.
Mechanisms of Lp(a) Contribution to Atherosclerosis
Lp(a) contributes to atherosclerosis through several mechanisms. One key factor is its ability to resist breakdown. This persistence allows it to remain in the bloodstream for extended periods, increasing its potential to contribute to plaque formation. Additionally, Lp(a) can stimulate inflammation and oxidative stress, further damaging the arterial walls and promoting the accumulation of cholesterol and other substances.
Cardiovascular Diseases Associated with High Lp(a) Levels
High Lp(a) levels are implicated in a variety of cardiovascular diseases. These include coronary artery disease (CAD), a leading cause of heart attack and stroke. Furthermore, high Lp(a) can contribute to stroke, which can lead to neurological deficits and long-term disability. Peripheral artery disease (PAD), a condition affecting blood vessels outside the heart and brain, is also linked to elevated Lp(a) levels.
Impact of Lp(a) on Different Cardiovascular Outcomes
| Cardiovascular Outcome | Potential Impact of High Lp(a) |
|---|---|
| Coronary Artery Disease | High Lp(a) levels can accelerate the development and progression of coronary artery disease by promoting the accumulation of plaque in the coronary arteries. This can lead to reduced blood flow to the heart, potentially resulting in angina, heart attack, or even sudden cardiac death. |
| Stroke | Elevated Lp(a) levels are linked to an increased risk of stroke, potentially by contributing to the formation of blood clots or by promoting the narrowing of blood vessels in the brain. This can result in various neurological impairments. |
| Peripheral Artery Disease | High Lp(a) levels can contribute to the development of PAD, which causes reduced blood flow to the extremities. This can lead to pain, numbness, cramping, and even tissue damage in the affected areas. In severe cases, it can necessitate amputation. |
Comparison of Lp(a) Effects on Different Blood Vessels
The effects of Lp(a) on different blood vessels are largely similar, centered around its contribution to atherosclerosis. While the specific manifestations of the disease can vary depending on the location of the affected blood vessels, the underlying mechanisms are comparable. In coronary arteries, high Lp(a) can lead to heart attack. In cerebral arteries, it can contribute to stroke.
In peripheral arteries, it can lead to PAD. The primary difference lies in the location and consequence of the atherosclerotic process.
Lp(a) Measurement and Testing
Determining lipoprotein(a) (Lp(a)) levels is crucial for assessing cardiovascular risk. Accurate measurement methods are vital for reliable interpretation and effective clinical management. This process involves various techniques, each with strengths and limitations, that provide insights into individual patient risk profiles.
Methods for Measuring Lp(a) Levels
Lp(a) measurement relies on various laboratory techniques, each with unique characteristics. These methods primarily focus on detecting the Lp(a) particle in blood samples. Immunological assays, often employing monoclonal antibodies specific to Lp(a), are widely used. These assays are designed to identify and quantify Lp(a) molecules based on their unique characteristics, ensuring accurate results. More sophisticated methods, such as enzyme-linked immunosorbent assays (ELISA), offer higher sensitivity and specificity, facilitating more precise quantification of Lp(a) levels.
Clinical Significance of Lp(a) Testing
Lp(a) testing holds significant clinical importance. Elevated Lp(a) levels are linked to a heightened risk of cardiovascular disease, including coronary artery disease, stroke, and peripheral artery disease. The test results are valuable for risk stratification and guiding preventive measures. Individuals with elevated Lp(a) levels might benefit from lifestyle modifications, medication, or closer monitoring to mitigate potential cardiovascular risks.
Units for Reporting Lp(a) Results
Lp(a) results are typically reported in mg/dL. This unit represents the concentration of Lp(a) in milligrams per deciliter of blood. Understanding the specific units used is crucial for interpreting the results correctly. A reference range, usually provided by the laboratory performing the test, is essential to determine if the individual’s Lp(a) level falls within the healthy range or indicates an elevated risk.
Lipoprotein (a), or Lp(a), cholesterol is a type of bad cholesterol that’s been linked to heart disease. While the exact role it plays in the complex web of health issues is still being researched, it’s a significant factor in cardiovascular health. The ongoing debate surrounding Israel’s expansion of settlements in the West Bank here highlights the interconnectedness of global issues and personal health choices.
Ultimately, understanding Lp(a) levels is a crucial aspect of proactive health management.
Factors Influencing Lp(a) Levels, What is lipoprotein lpa cholesterol
Several factors can influence Lp(a) levels. Genetics play a significant role, as Lp(a) levels are largely determined by inherited factors. Age, gender, and certain medical conditions can also affect Lp(a) levels. Furthermore, lifestyle factors, such as diet and exercise, might have a modest influence on Lp(a) levels. It’s important to note that these influences can vary from person to person, and comprehensive evaluation is needed to interpret Lp(a) levels in a specific context.
Lipoprotein (a), or Lp(a), cholesterol is a type of cholesterol that’s been linked to heart disease risk. Recent studies are exploring the potential impact of various dietary factors on Lp(a) levels, but the connection between this cholesterol and the plight of South African refugees, like those fleeing Haiti to find safety in South Africa, is still largely unknown. While the complexities of south africa haiti white refugees are undeniably significant, understanding the factors influencing Lp(a) levels remains a crucial area of research for improving cardiovascular health.
Accuracy and Limitations of Lp(a) Testing Methods
Different methods for measuring Lp(a) levels exhibit varying degrees of accuracy and have inherent limitations. The choice of method often depends on the specific needs of the clinical setting and the desired level of precision.
| Method | Accuracy | Limitations |
|---|---|---|
| Immunoturbidimetric Assays | Generally accurate and widely used. | Potential for interference from other blood components and variability between laboratories. |
| ELISA (Enzyme-linked Immunosorbent Assay) | High sensitivity and specificity, offering detailed analysis. | Can be more complex and time-consuming compared to other methods. Cost can be a factor. |
Management and Treatment Strategies
Managing elevated Lp(a) levels is a complex issue, as there’s currently no medication specifically designed to lower Lp(a) levels. Treatment strategies primarily focus on reducing overall cardiovascular risk factors, which can indirectly impact Lp(a) levels and the associated risk of cardiovascular disease. This often involves a combination of lifestyle modifications and, in some cases, medication to manage other risk factors.
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing cardiovascular risk factors, and consequently, Lp(a) levels. These modifications often improve overall health and can positively influence Lp(a) levels, although the exact mechanisms are not fully understood. Focusing on a healthy lifestyle is beneficial even if Lp(a) levels aren’t significantly elevated.
- A balanced diet rich in fruits, vegetables, and whole grains, while limiting saturated and trans fats, cholesterol, and sodium, can positively influence Lp(a) levels.
- Regular physical activity, such as brisk walking, jogging, swimming, or cycling, can help lower Lp(a) levels and overall cardiovascular risk. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week.
- Maintaining a healthy weight is essential for managing Lp(a) and overall cardiovascular health. Obesity is a significant risk factor for elevated Lp(a) levels. Sustainable weight loss, achieved through a combination of diet and exercise, can have a positive impact on Lp(a) levels.
- Quitting smoking is a crucial step in reducing cardiovascular risk. Smoking significantly increases the risk of cardiovascular disease, regardless of Lp(a) levels. Stopping smoking immediately can improve overall health and lower cardiovascular risk factors.
- Adequate sleep is essential for overall health and can indirectly impact Lp(a) levels by regulating various physiological processes. Aim for 7-9 hours of quality sleep each night to maintain good health and reduce cardiovascular risk factors.
Pharmacological Interventions
While no specific drugs target Lp(a) reduction, medications used to treat other cardiovascular risk factors may indirectly affect Lp(a) levels or reduce overall cardiovascular risk. Statins, for example, are frequently used to lower LDL cholesterol, which can also impact Lp(a) levels, although the effect is not consistent.
- Statins, often prescribed to lower LDL cholesterol, have shown some potential in reducing Lp(a) levels, though the effect is not always consistent and can vary depending on the individual and the specific statin used. The reduction in Lp(a) is usually modest.
- Other medications, such as niacin, might have a minor effect on Lp(a) levels. However, their efficacy and potential side effects need to be carefully considered by a healthcare professional. Niacin can interact with other medications, and its use should be evaluated in the context of other risk factors.
Limitations of Available Treatments
Currently, there are no medications specifically designed to target Lp(a) reduction. While lifestyle modifications and some medications might indirectly affect Lp(a) levels, the effectiveness can vary significantly between individuals. More research is needed to develop targeted therapies.
- The lack of specific Lp(a)-lowering drugs poses a significant limitation. The effectiveness of indirect methods is variable, making precise management challenging.
- The complex interplay between Lp(a) and other cardiovascular risk factors makes isolating the impact of Lp(a) reduction challenging. Other factors often need to be addressed simultaneously for comprehensive risk management.
- The long-term effects of different treatment strategies on Lp(a) levels are still being investigated. More extensive studies are needed to provide a clearer picture of the long-term impact.
Genetic Factors and Lp(a)
Lp(a) levels are significantly influenced by genetics. Understanding the role of inherited factors is crucial for assessing individual risk and developing personalized strategies for managing Lp(a). The interplay between genes and lifestyle choices plays a critical part in determining an individual’s Lp(a) levels.The complex genetic mechanisms underlying Lp(a) levels are not fully understood, but studies suggest that multiple genes contribute to the variation in Lp(a) concentrations among individuals.
This complexity makes it challenging to pinpoint a single gene as the sole determinant of Lp(a) levels. However, ongoing research continues to unravel the intricate genetic pathways involved.
Genes Associated with Lp(a) Variation
Several genes have been linked to variations in Lp(a) levels. The most prominent gene is the LPA gene, which codes for the apolipoprotein(a) component of Lp(a). Variations within this gene are strongly associated with Lp(a) levels. Other genes, including those involved in lipid metabolism and inflammation, likely contribute to the overall genetic influence on Lp(a).
Inheritance Patterns of Lp(a) Levels
Lp(a) levels follow a complex pattern of inheritance. While the exact inheritance pattern isn’t completely clear-cut, it’s generally understood that Lp(a) levels exhibit a polygenic inheritance pattern. This means that multiple genes, each with a small effect, contribute to the overall Lp(a) level in an individual. This polygenic nature is a common feature in many complex traits.
Family History and Lp(a) Levels
A family history of high Lp(a) levels is a significant risk factor. Individuals with family members who have elevated Lp(a) and cardiovascular disease are at a higher risk themselves. This suggests a strong genetic predisposition to elevated Lp(a). The inheritance patterns within families can influence Lp(a) levels, showcasing the genetic impact on an individual’s predisposition. Examples include observing elevated Lp(a) levels in multiple siblings or parents, suggesting a familial tendency.
Correlation between Genetic Variations and Lp(a) Levels
The following table demonstrates potential correlations between specific genetic variations and Lp(a) levels. Note that the specific correlations and their strength can vary among different populations and studies. Ongoing research is constantly refining our understanding of these correlations.
| Genetic Variation | Correlation with Lp(a) Levels |
|---|---|
| LPA gene variations (e.g., specific SNPs) | Strong correlation, often associated with higher Lp(a) levels. |
| Genes involved in lipid metabolism (e.g., APOE, LDLR) | Moderate correlation, influenced by the specific variations and their interaction with other genes. |
Public Health Implications
High levels of lipoprotein(a), or Lp(a), cholesterol pose significant public health concerns due to its strong association with cardiovascular disease (CVD). Understanding its prevalence, impact, and potential preventative measures is crucial for developing effective public health strategies. This section delves into the broader implications of Lp(a) on populations and the importance of raising awareness.
Prevalence of High Lp(a) Levels
Lp(a) levels vary considerably among different populations. Genetic predisposition plays a key role, with some ethnic groups exhibiting higher average Lp(a) levels than others. Studies have shown that individuals of certain ancestries may have a greater likelihood of elevated Lp(a) concentrations, potentially increasing their risk for CVD. Factors such as age, gender, and lifestyle choices also contribute to the variability in Lp(a) levels within a population.
Potential Impact of High Lp(a) on Public Health
High Lp(a) levels contribute significantly to the global burden of cardiovascular disease. This translates into increased healthcare costs, lost productivity, and diminished quality of life for affected individuals and their families. The cumulative effect of high Lp(a) across large populations can have a substantial impact on public health systems, demanding greater resources for diagnosis, treatment, and long-term management of CVD.
Importance of Raising Public Awareness about Lp(a)
Public awareness campaigns about Lp(a) and its link to CVD are vital for early detection and preventive measures. Educating the public about risk factors, lifestyle modifications, and available diagnostic tools can empower individuals to take proactive steps towards maintaining cardiovascular health. Promoting awareness can help individuals understand their personal risk and make informed decisions about their health.
Long-Term Health Implications of High Lp(a) Levels
High Lp(a) levels are associated with a significantly increased risk of developing various cardiovascular diseases, including coronary artery disease, stroke, and peripheral artery disease. These conditions can lead to serious health complications, such as heart attacks, heart failure, and reduced mobility. Long-term health implications also include the potential for premature mortality, impacting individuals’ overall life expectancy.
Preventative Measures
Effective preventative measures for high Lp(a) levels encompass lifestyle modifications and potential future therapeutic interventions. Maintaining a healthy diet, engaging in regular physical activity, and avoiding tobacco use are fundamental steps. Addressing underlying conditions like high blood pressure and high cholesterol is crucial for managing cardiovascular risk factors. Further research into potential therapies to lower Lp(a) levels is an ongoing area of investigation, offering potential preventative strategies for the future.
Final Summary
In summary, lipoprotein (a) cholesterol, or Lp(a), is a significant factor in cardiovascular health. While genetics play a role in its levels, understanding the risks associated with elevated Lp(a) and the available management strategies is crucial. Testing, lifestyle modifications, and potential treatments can help manage Lp(a) and mitigate the risk of related health complications. Further research and advancements in understanding Lp(a) are essential for improving public health outcomes.