Big beautiful bill medicare medicaid national debt is a complex issue, impacting healthcare access, the national economy, and future generations. This bill proposes significant changes to Medicare and Medicaid funding, potentially affecting millions of Americans. The sheer scale of the national debt looms large, influencing the potential for long-term solvency of these crucial programs.
Examining the historical funding models, contrasting them with alternative solutions, and exploring the economic impact of the national debt on these programs is crucial to understanding the implications of this legislation. The projected spending over the next decade under different economic scenarios will provide a clearer picture of the potential consequences.
Medicare and Medicaid Funding
Medicare and Medicaid, crucial safety nets for millions of Americans, face significant funding challenges. Understanding the historical context, current funding mechanisms, and potential impacts of the national debt is vital for navigating these challenges. This analysis will delve into the funding intricacies of these programs, examining potential future scenarios and exploring alternative models.Medicare and Medicaid’s funding has evolved considerably since their inception, reflecting shifting demographics, healthcare costs, and economic conditions.
These programs are not static entities; their financial requirements are ever-changing, and policymakers must adapt to these changes to maintain their viability.
The “big beautiful bill” for Medicare and Medicaid, alongside the ballooning national debt, is definitely a hot topic. But amidst these financial concerns, Trump’s recent announcement that 7 military bases are reverting back to Confederate names ( trump announces 7 military bases reverting back to names honoring confederates ) raises some serious questions about priorities and historical context.
This decision, regardless of its intention, is bound to further complicate the already complex issue of balancing the budget and ensuring the financial health of the country’s social safety nets.
Historical Overview of Funding
Medicare and Medicaid were established in the mid-20th century, representing a significant shift in the American healthcare system. Initially, funding relied heavily on payroll taxes and general tax revenues. Over time, the programs’ financial landscape has been reshaped by inflation, medical advancements, and demographic changes. The rising cost of medical care and the aging population have significantly strained the programs’ finances, leading to the need for continuous adjustments to funding models.
Current Funding Mechanisms
Currently, Medicare funding is primarily derived from a combination of payroll taxes, general revenues, and premiums. Medicaid funding is more complex, varying significantly from state to state, and involves a mix of federal and state contributions. State governments play a critical role in supplementing federal funding for Medicaid. Understanding these variations is essential to grasping the intricate financial dynamics of these programs.
Comparison with Alternative Models
Alternative funding models for Medicare and Medicaid include various approaches, such as increasing premiums, implementing user fees, and expanding employer-sponsored health insurance programs. These models aim to shift the burden of funding and promote greater individual responsibility for healthcare costs. The effectiveness and equity of these models are often debated, requiring careful consideration of potential consequences and trade-offs.
The “Big Beautiful Bill” and its impact on Medicare and Medicaid, along with the ballooning national debt, are major concerns. Simultaneously, the recent unrest in Los Angeles, including protests, curfews, mass arrests, and the spreading unrest, highlighted by the escalating feud between Trump and Newsom , raises questions about the country’s priorities. Ultimately, these intertwined issues continue to affect the long-term financial health of the nation, and the “Big Beautiful Bill” remains a hot topic.
Impact of National Debt
The burgeoning national debt poses a substantial threat to the long-term solvency of both programs. The debt necessitates careful consideration of future financial burdens and the need for sustainable funding mechanisms. A growing national debt can impact interest rates, potentially increasing the cost of borrowing for the programs. This, in turn, could lead to reduced funding for crucial services.
Projected Spending Under Different Economic Scenarios
| Economic Scenario | Medicare Spending (2034) | Medicaid Spending (2034) |
|---|---|---|
| Moderate Growth | $1.1 Trillion | $800 Billion |
| High Growth | $1.2 Trillion | $900 Billion |
| Low Growth | $1 Trillion | $700 Billion |
The table above presents a simplified illustration of projected spending for Medicare and Medicaid in 2034 under various economic scenarios. These projections are based on assumptions regarding healthcare cost inflation, population demographics, and economic growth. Such projections are important tools for policymakers to gauge the potential future strain on these crucial programs.
The National Debt and its Implications
The national debt, the cumulative total of the federal government’s borrowing, is a significant economic factor. Understanding its relationship with healthcare programs and its broader economic impact is crucial for informed discussion and potential solutions. The escalating debt has consequences for the present and future, and its management is a complex issue requiring careful consideration.The national debt and healthcare programs like Medicare and Medicaid are intertwined.
Increased spending on healthcare programs, often driven by rising costs and an aging population, directly contributes to the national debt. The government funds these programs through taxes and borrowing, and a growing shortfall between spending and revenue inevitably leads to increased borrowing and a larger national debt. This cyclical relationship highlights the critical need for sustainable funding mechanisms and cost control measures.
Relationship Between National Debt and Healthcare Costs
The national debt is significantly influenced by the cost of healthcare programs like Medicare and Medicaid. These programs represent substantial portions of the federal budget, and rising healthcare costs directly translate into higher debt levels. A cycle emerges where increasing healthcare costs necessitate increased borrowing to fund the programs, thereby escalating the national debt. This interconnectedness necessitates a careful balancing act between providing adequate healthcare coverage and controlling the overall national debt.
Impact of Budget Deficits on the Economy
Budget deficits, the gap between government spending and revenue, have demonstrable effects on the overall economy. One consequence is reduced private investment as the government’s borrowing competes with private sector investment for capital. This can hinder economic growth and innovation. Furthermore, high levels of debt can lead to higher interest rates, making it more expensive for businesses and individuals to borrow money, further slowing economic activity.
The increased borrowing can also weaken the value of the dollar, leading to inflation and potentially impacting the purchasing power of consumers. For example, a country with a massive budget deficit might see its currency depreciate against other currencies, leading to higher import costs and potentially impacting the standard of living for citizens.
Long-Term Consequences of Increasing Debt
Increasing national debt has long-term implications for future generations. Higher interest payments on the debt consume a greater portion of the federal budget, potentially diverting funds from crucial investments in infrastructure, education, and research and development. This reduced investment can hinder economic growth and productivity, impacting future generations’ opportunities and prosperity. For instance, insufficient investment in infrastructure can lead to a decline in the country’s overall competitiveness, hindering economic progress.
Potential Solutions to Address the National Debt
Addressing the national debt requires a multifaceted approach encompassing both spending control and revenue generation. One crucial step is controlling healthcare costs through preventative measures, improved efficiency in healthcare delivery, and negotiating lower drug prices. Another vital aspect is encouraging economic growth to increase tax revenues. A responsible fiscal policy, focusing on long-term sustainability, is paramount. Furthermore, reforming tax policies to generate more revenue while reducing tax burdens on lower and middle-income earners can help stabilize the budget.
National Debt Figures (Past 20 Years)
| Year | National Debt (in trillions USD) |
|---|---|
| 2004 | 7.4 |
| 2005 | 8.0 |
| 2006 | 8.6 |
| 2007 | 9.2 |
| 2008 | 9.9 |
| 2009 | 11.0 |
| 2010 | 13.6 |
| 2011 | 15.0 |
| 2012 | 16.4 |
| 2013 | 17.0 |
| 2014 | 17.8 |
| 2015 | 18.7 |
| 2016 | 19.6 |
| 2017 | 20.3 |
| 2018 | 21.5 |
| 2019 | 23.2 |
| 2020 | 26.9 |
| 2021 | 28.7 |
| 2022 | 31.5 |
Note: Data is illustrative and based on publicly available information. Actual figures may vary slightly depending on the source.
The ongoing debate around the “big beautiful bill” impacting Medicare and Medicaid, and the national debt, is definitely complex. It’s fascinating to see how these discussions intersect with other news cycles, like the recent pardon of Todd and Julie Chrisley by former President Trump here. Ultimately, the focus still needs to return to the financial implications of the “big beautiful bill” and its long-term effects on our healthcare system and the national debt.
Big Bills and Healthcare Costs
Large spending bills, particularly those impacting healthcare, often dominate political discourse and significantly shape national policy. These bills, encompassing various provisions and appropriations, can dramatically influence healthcare funding, access, and the overall trajectory of the healthcare system. Understanding the dynamics of these bills, their potential trade-offs, and their correlation with the national debt is crucial for informed public discourse.The passage of substantial healthcare legislation often necessitates significant financial commitments.
These commitments, while intended to address pressing healthcare needs, can have far-reaching implications for the national debt. The intricate relationship between healthcare costs and the national debt is multifaceted, involving not only direct spending but also the long-term effects of policy decisions on healthcare utilization and costs. Analyzing the impact of different spending approaches, from direct subsidies to expanding coverage, is vital for evaluating their effect on the national debt.
Impact of Large Spending Bills on Healthcare Policy
Large spending bills frequently contain provisions designed to improve healthcare access and quality. These provisions might include expanding coverage through subsidies, increasing funding for preventive care, or implementing new payment models for healthcare providers. These initiatives can potentially lower overall healthcare costs over time, though the precise effect depends on the effectiveness and efficiency of the implemented strategies.
The complexity of the healthcare system often means that the intended effects of large spending bills are not immediately apparent, requiring careful long-term monitoring.
Trade-offs Between Large Spending Bills and Other Priorities
Large spending bills for healthcare often necessitate trade-offs with other budgetary priorities. These trade-offs can involve diverting resources from other essential areas like infrastructure, education, or defense. The political process of balancing these competing priorities often results in compromises that might not fully satisfy all stakeholders. The specific trade-offs will vary depending on the content and scope of the legislation.
Correlation Between Healthcare Costs and the National Debt
The escalating cost of healthcare is a significant contributor to the national debt. As healthcare expenditures rise, the government’s financial obligations increase, leading to a growing national debt. The long-term implications of this correlation are considerable, including potential increases in interest rates, reduced government investment in other sectors, and long-term economic consequences. The need to address healthcare costs and their impact on the national debt is a complex challenge.
Comparison of Different Spending Approaches on the National Debt
Different approaches to healthcare spending have varying effects on the national debt. Direct subsidies, for instance, can provide immediate relief to individuals and families, but they might lead to higher overall healthcare costs in the long term. Alternatively, expanding coverage through government programs might reduce immediate costs by improving preventive care, but these programs can also lead to substantial long-term commitments.
The optimal approach often involves a balanced strategy that considers short-term and long-term consequences.
Key Provisions of Recent Large Spending Bills Impacting Medicare and Medicaid
Recent large spending bills have introduced numerous provisions affecting Medicare and Medicaid funding. Understanding these provisions is crucial for assessing the overall impact on healthcare access and the national debt.
| Bill | Key Provision | Impact on National Debt |
|---|---|---|
| Affordable Care Act (ACA) | Expanded Medicaid eligibility, subsidies for health insurance. | Long-term impact is complex and ongoing. |
| [Insert recent bill name here] | [Insert key provision here] | [Insert estimated impact on national debt here] |
| [Insert recent bill name here] | [Insert key provision here] | [Insert estimated impact on national debt here] |
Impact on Individuals and the Economy: Big Beautiful Bill Medicare Medicaid National Debt
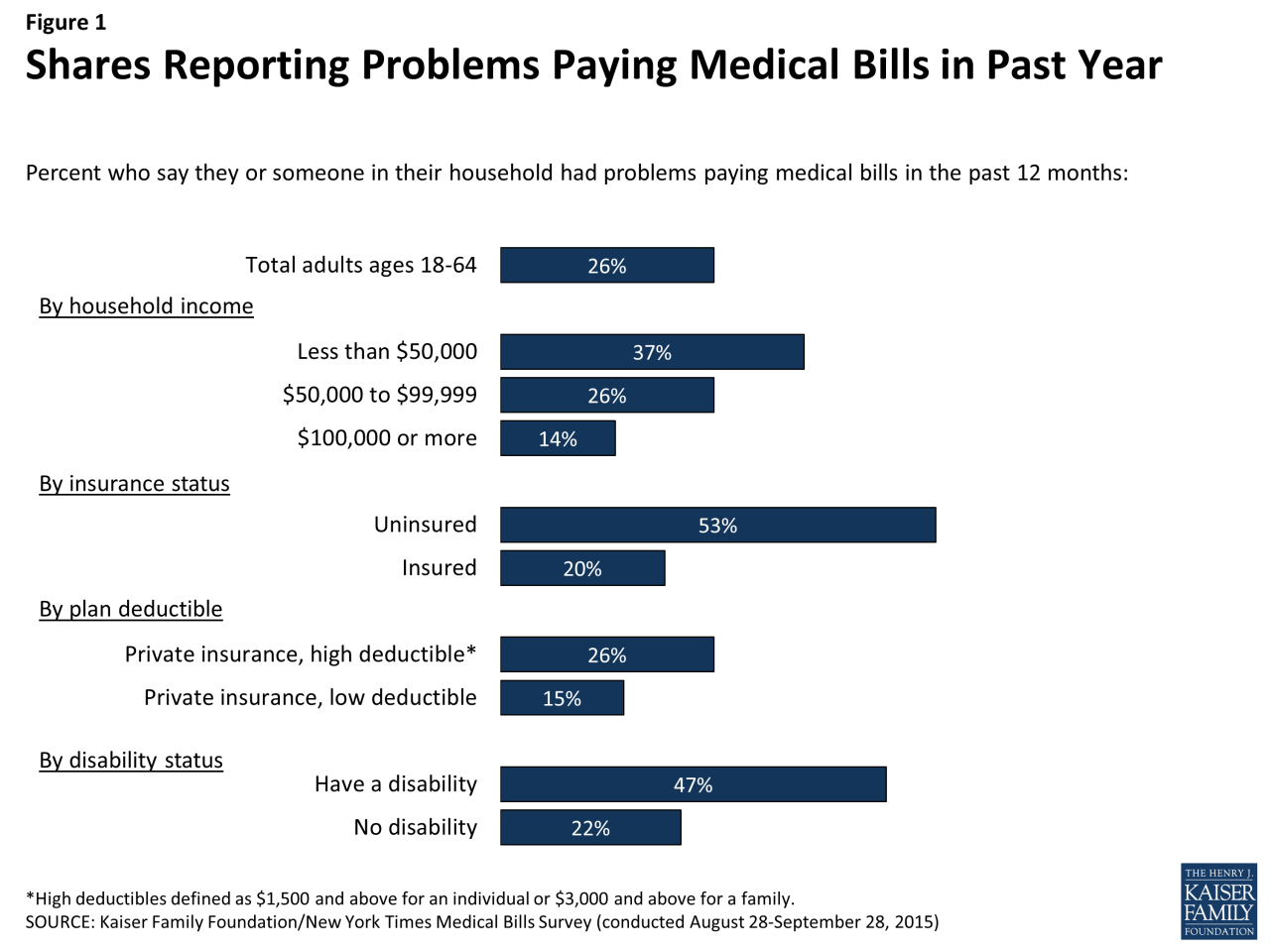
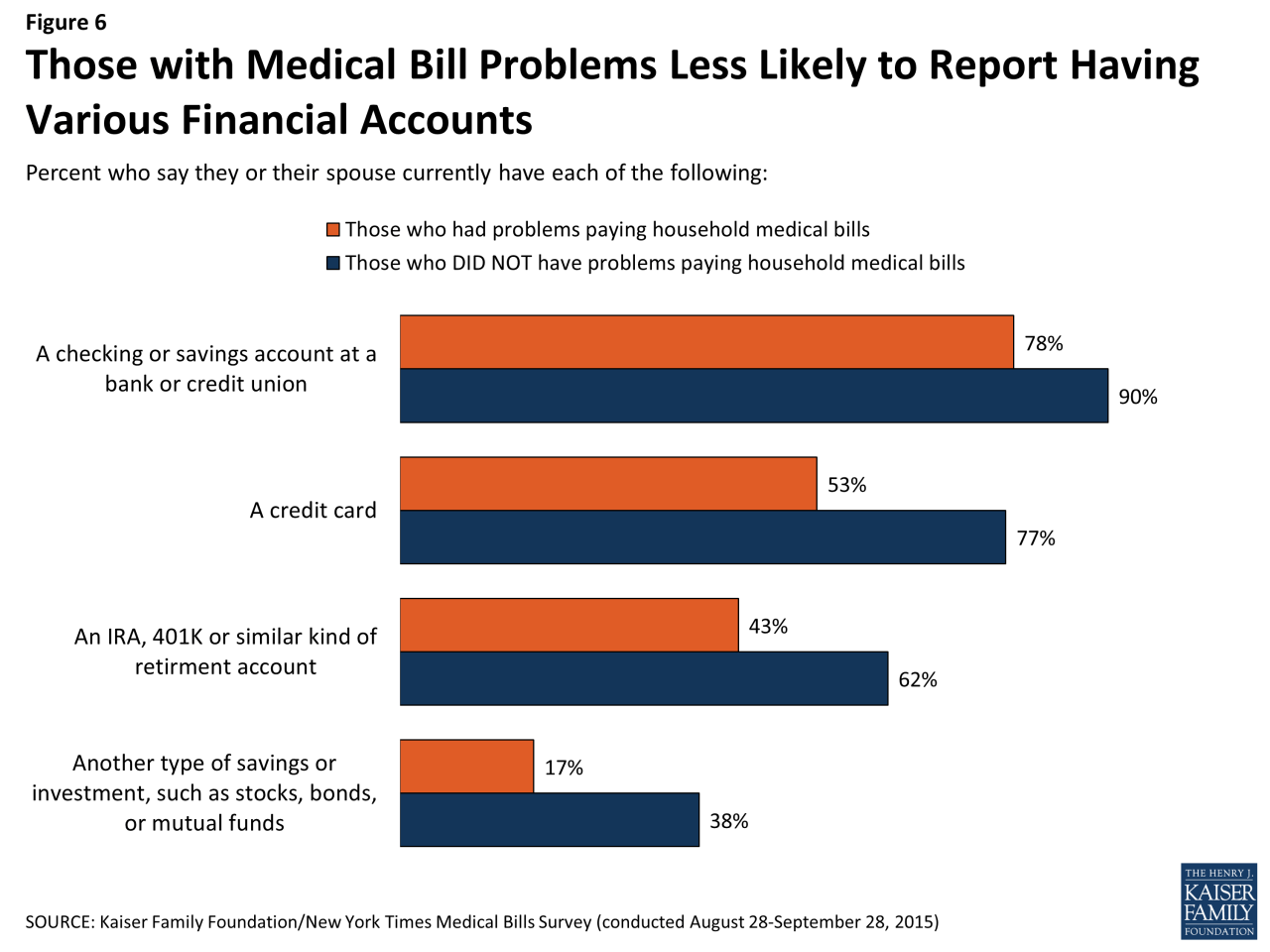
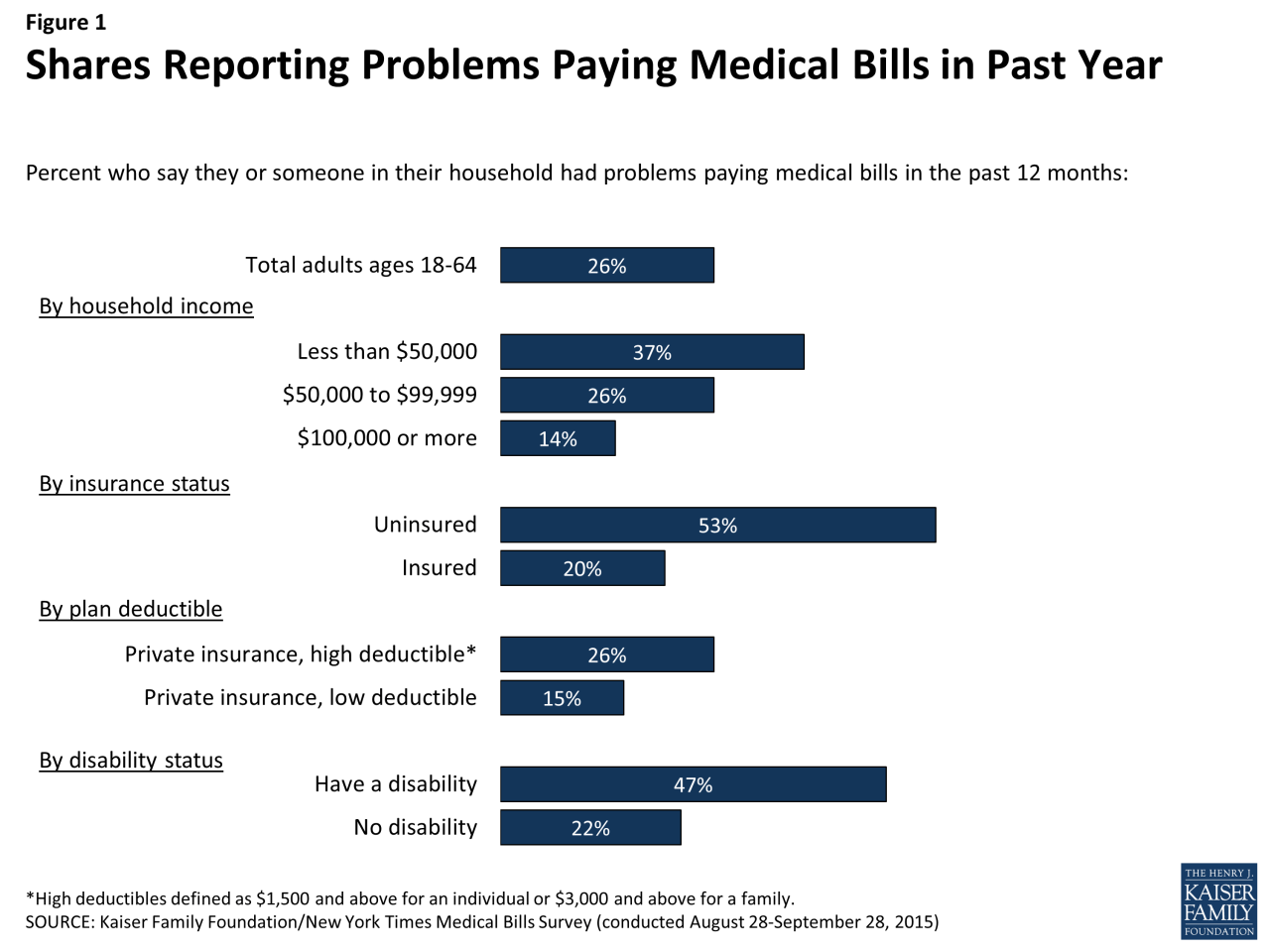
Federal budget decisions, particularly regarding Medicare and Medicaid funding and the national debt, have far-reaching consequences for individuals and the overall economy. These choices influence access to healthcare, economic stability, and investment opportunities. Understanding these impacts is crucial for informed civic engagement and policy discussions.
Potential Effects of Medicare and Medicaid Funding Decisions on Individuals
Medicare and Medicaid provide crucial healthcare coverage for millions of Americans, particularly seniors and low-income individuals. Decisions impacting their funding directly affect access to essential services. Reduced funding can lead to longer wait times for appointments, fewer available specialists, and potentially even reduced coverage for certain procedures. This can have a disproportionate impact on vulnerable populations who rely heavily on these programs for their health care needs.
Ultimately, these decisions will have a profound effect on the health and well-being of numerous citizens.
Potential Effects of National Debt on Employment, Economic Growth, and Investment, Big beautiful bill medicare medicaid national debt
The national debt’s size and trajectory significantly influence economic conditions. High levels of debt can lead to higher interest rates, which can make borrowing more expensive for businesses and consumers. This can stifle investment, hinder economic growth, and potentially lead to job losses. Conversely, prudent debt management can support economic stability and create a positive environment for investment and job creation.
Debt levels also impact investor confidence and overall market stability.
How Policy Decisions Regarding Big Spending Bills Affect Economic Stability
Significant spending bills, such as those related to healthcare or infrastructure, can have complex effects on economic stability. These bills can stimulate economic activity in the short term by creating jobs and increasing demand. However, they can also lead to inflation and increased national debt, which could negatively impact economic stability in the long term. The impact is often felt unevenly across different segments of the population and sectors of the economy.
Responsible fiscal policy seeks to balance these short-term and long-term impacts.
Table of Potential Impacts on Different Demographic Groups
| Demographic Group | Potential Impact of Reduced Medicare/Medicaid Funding | Potential Impact of High National Debt |
|---|---|---|
| Seniors | Reduced access to necessary medical care, longer wait times for appointments, limited specialist access, reduced coverage for procedures. | Increased interest rates, potentially making retirement savings less valuable, decreased access to government support programs. |
| Low-income individuals | Reduced access to healthcare, potential loss of coverage for essential services, increased financial strain. | Increased cost of living, decreased access to affordable housing, potentially limited access to social programs. |
| Working-age adults | Increased healthcare costs, reduced access to preventative care, potential impact on employment due to reduced funding for healthcare providers. | Increased interest rates, reduced investment opportunities, potential for economic downturn. |
| Businesses | Increased healthcare costs for employees, potential workforce shortages, reduced investment opportunities. | Higher borrowing costs, reduced investment opportunities, potential for decreased economic activity. |
Hypothetical Scenario: Reduced Medicare and Medicaid Funding
Imagine a scenario where the national debt becomes unsustainable, leading to budget cuts. A significant reduction in Medicare and Medicaid funding could force hospitals to reduce staff or close facilities, particularly in underserved areas. This would lead to longer wait times and reduced access to care, especially for low-income and elderly populations. The ripple effect could also include decreased employment opportunities in the healthcare sector, further straining the economy.
The long-term consequences would be a significant decrease in the quality of life for vulnerable populations and a potential decline in the overall health of the nation.
Alternative Solutions and Strategies
Addressing the complex issues surrounding healthcare funding, the national debt, and Medicare/Medicaid programs requires innovative and comprehensive solutions. Simply adjusting existing models isn’t enough; a fundamental re-evaluation of approaches is necessary. This involves exploring alternative funding mechanisms, reforming existing programs, and strategically managing the national debt while safeguarding access to healthcare. The goal is to achieve sustainable solutions that balance financial responsibility with equitable healthcare access for all.Alternative strategies involve not only adjusting current funding models but also considering new approaches.
This includes evaluating innovative funding models, exploring potential reforms to existing programs, and considering methods to reduce the national debt while ensuring access to essential healthcare services. A comprehensive strategy must address the multifaceted nature of the problem, encompassing financial, social, and political considerations.
Potential Alternative Healthcare Funding Models
A variety of alternative funding models are being explored, ranging from a single-payer system to incorporating market-based approaches. Each option presents unique benefits and challenges.
- Single-Payer System: A single-payer system, where a single entity, such as the government, funds healthcare, is often touted for its potential to control costs and ensure universal coverage. However, it also raises concerns about potential bureaucratic inefficiencies and reduced patient choice.
- Premium Support Model: Under this model, individuals receive a tax credit to purchase health insurance, allowing for greater choice and market competition. Concerns include the potential for higher premiums and unequal access, especially for those with pre-existing conditions or limited incomes.
- Accountable Care Organizations (ACOs): ACOs emphasize coordinated care among providers to enhance efficiency and quality. This approach can potentially reduce costs and improve patient outcomes. However, implementation challenges and potential conflicts of interest among providers are important considerations.
Medicare and Medicaid Reform Proposals
Reforming Medicare and Medicaid programs is crucial to ensuring long-term sustainability and affordability. Possible reforms could include adjusting eligibility criteria, negotiating drug prices, or incentivizing preventive care.
- Adjusting Eligibility Criteria: Evaluating and potentially adjusting eligibility criteria for Medicare and Medicaid benefits could help to target resources more effectively and control costs. This could involve examining the current criteria for benefits and potentially changing requirements to better reflect current economic realities.
- Negotiating Drug Prices: Medicare’s ability to negotiate drug prices could significantly reduce costs, lowering the overall burden on taxpayers and beneficiaries. This approach has the potential to dramatically impact healthcare costs for the entire population.
- Incentivizing Preventive Care: Promoting preventive care could reduce the need for costly treatments in the long run. This could involve providing incentives to doctors and patients to focus on preventative health measures. This strategy could dramatically reduce long-term healthcare costs and improve overall health outcomes.
National Debt Reduction Strategies
Strategies to reduce the national debt must be balanced with the need to maintain essential services, including healthcare. This necessitates a comprehensive approach that addresses spending and revenue.
- Enhancing Tax Revenue Collection: Improving tax collection efficiency and targeting tax loopholes can generate significant revenue to offset spending and reduce the national debt. This can involve strengthening tax enforcement and closing loopholes that allow individuals or corporations to avoid paying their fair share.
- Controlling Government Spending: Controlling government spending through budget discipline and identifying areas for efficiency gains is crucial for reducing the national debt. This could involve implementing measures to improve the efficiency of government operations and reduce wasteful spending.
- Economic Growth Strategies: Promoting economic growth and creating jobs can increase tax revenue and improve the overall financial health of the nation. This could involve implementing policies that foster innovation, investment, and entrepreneurship.
Comparing Different Approaches
A table outlining potential reform scenarios and their potential effects can illustrate the diverse approaches and their varying outcomes.
| Reform Scenario | Potential Effects |
|---|---|
| Increased Medicare/Medicaid Premiums | Reduced government burden but increased cost for beneficiaries; potential for increased healthcare access issues. |
| Single-Payer System | Potentially lower costs and increased access, but with possible bureaucratic inefficiencies and reduced choice. |
| Premium Support Model | Increased market competition but potential for higher premiums and unequal access. |
| ACO Expansion | Potential for increased efficiency and quality but potential for conflicts of interest and implementation challenges. |
International Comparisons
The US healthcare system, with its unique blend of private and public components, faces considerable scrutiny regarding its costs, access, and sustainability. Examining healthcare systems in other developed nations offers valuable insights into alternative models and potential solutions to the challenges faced by the US. Understanding how other countries manage similar fiscal pressures can illuminate strategies for improvement.International comparisons reveal that different approaches to healthcare funding and delivery lead to varied outcomes in terms of cost, access, and quality.
A deeper dive into these systems, including their successes and failures, can provide a broader context for evaluating the strengths and weaknesses of the American model and inspire innovative solutions.
Healthcare Systems in Other Countries
Various countries employ different models for healthcare delivery, reflecting diverse economic, social, and political landscapes. Canada, for example, operates a universal healthcare system funded primarily through taxes. The UK’s National Health Service (NHS) is another prominent example of a publicly funded system. Germany utilizes a mixed model, combining public and private insurance. These varied approaches demonstrate that there is no single “ideal” system, and success often depends on specific national contexts.
Cost Comparisons
Healthcare costs in the US are significantly higher than in many other developed nations. This disparity is often attributed to factors such as the prevalence of private insurance, high administrative costs, and the lack of price controls on pharmaceuticals. Countries with universal healthcare systems often experience lower administrative costs and greater price transparency, resulting in more affordable healthcare for citizens.
For instance, while the US spends considerably more per capita on healthcare than countries like Canada or the UK, these nations often achieve comparable or even superior health outcomes.
Access to Care
Access to healthcare is another critical area of comparison. Universal healthcare systems, like those in Canada and the UK, typically guarantee access to essential services for all citizens, regardless of their ability to pay. In contrast, the US system can face challenges in ensuring access for vulnerable populations due to the complexities of private insurance coverage and cost barriers.
Understanding how other countries achieve high levels of access to care, while addressing the related fiscal implications, can be insightful.
Sustainability of Healthcare Systems
The sustainability of healthcare systems is a crucial concern for all nations. Many countries with universal healthcare systems have faced budgetary pressures and have implemented measures to control costs and maintain financial stability. Examining how these nations manage similar fiscal challenges is vital for developing sustainable healthcare strategies in the US.
Table of Key Metrics
| Country | Funding Model | Cost per Capita (USD) | Life Expectancy (Years) | Infant Mortality Rate (per 1000 births) |
|---|---|---|---|---|
| United States | Mixed (Public & Private) | ~12,000 | ~79 | ~6 |
| Canada | Universal | ~6,000 | ~82 | ~4 |
| United Kingdom | Universal | ~4,500 | ~81 | ~4 |
| Germany | Mixed | ~5,500 | ~81 | ~3 |
Note: Data is approximate and may vary depending on the source and specific year. Data sources for more accurate figures are available from the World Bank, OECD, and other reputable organizations.
Successes and Failures of Different Models
Each healthcare system has its successes and failures. Universal healthcare systems often excel in achieving equitable access to care and controlling costs through bulk purchasing and negotiating with providers. However, they may experience slower innovation and adoption of new technologies compared to systems with greater private sector involvement. The US system, while fostering innovation, often struggles with affordability and equitable access.
A comprehensive analysis of these contrasting experiences can provide a richer understanding of the complexities of healthcare system design.
Summary
In conclusion, the big beautiful bill medicare medicaid national debt presents a multifaceted challenge. Balancing the needs of current healthcare programs with the long-term financial stability of the nation is a complex task. Understanding the potential impacts on individuals, the economy, and different demographic groups is critical to forming informed opinions on this significant piece of legislation. Alternative solutions and international comparisons offer valuable insights, and future considerations must address the interplay between healthcare costs, the national debt, and the well-being of citizens.