Climate change sleep apnea is emerging as a significant health concern, linking the escalating effects of global warming to a rise in sleep apnea cases. This growing problem isn’t just about disrupted sleep; it’s about a complex interplay between environmental factors and our respiratory health. We’ll explore how rising temperatures, air pollution, and extreme weather events are contributing to the development and worsening of sleep apnea, and how this disproportionately impacts vulnerable populations.
The physiological mechanisms behind this connection are multifaceted, with high temperatures directly impacting airway resistance and sleep quality. Air pollution, particularly particulate matter, inflames airways and exacerbates sleep apnea symptoms. We’ll examine the specific pollutants and weather patterns that are linked to sleep apnea, and how they disproportionately affect vulnerable groups like the elderly and children. A deeper look at these factors will help us understand the risk factors and the potential health consequences.
Introduction to the Link Between Climate Change and Sleep Apnea
Climate change is impacting human health in numerous ways, from increased heat-related illnesses to the spread of infectious diseases. A less discussed but equally concerning consequence is its potential influence on sleep apnea, a prevalent sleep disorder characterized by pauses in breathing during sleep. The rising temperatures, altered weather patterns, and increased air pollution linked to climate change can create a cascade of effects on our bodies, making sleep apnea more likely to develop or worsen.
Understanding this link is crucial for developing effective preventative measures and targeted interventions, particularly for vulnerable populations.
Potential Impacts of Climate Change on Human Health
Climate change significantly alters environmental conditions, leading to a variety of health concerns. Rising global temperatures, shifts in precipitation patterns, and increased frequency of extreme weather events directly affect human health. Heat waves, for instance, can exacerbate existing health conditions, and the spread of vector-borne diseases is also a major concern. The quality of our air, a key component of respiratory health, is also impacted.
Increased air pollution from wildfires and other sources can trigger or worsen respiratory illnesses, including asthma and chronic obstructive pulmonary disease (COPD). These impacts highlight the urgent need for climate action and adaptable strategies to protect human health.
Physiological Mechanisms Contributing to Sleep Apnea
The physiological mechanisms linking climate change to sleep apnea are multifaceted. Changes in temperature and humidity can affect airway resistance, making it harder for air to flow through the respiratory system. Elevated temperatures can also cause vasodilation (widening of blood vessels), which may lead to a reduction in the efficiency of breathing muscles. These changes, in combination with other environmental factors, can exacerbate the symptoms of sleep apnea, potentially triggering or worsening the condition.
Furthermore, individuals with existing sleep apnea may find their symptoms worsened by these changes.
Environmental Factors Affecting Sleep Quality and Respiratory Function
Environmental factors such as air pollution and extreme temperatures significantly impact sleep quality and respiratory function. Air pollution, whether from industrial sources or wildfires, can irritate the airways and make breathing difficult, potentially leading to sleep disturbances and exacerbating existing sleep apnea. Extreme temperatures, particularly heat waves, can also impair sleep quality and reduce the efficiency of the respiratory system, further contributing to sleep apnea symptoms.
The combination of these factors can create a vicious cycle, making individuals more susceptible to developing or experiencing worse sleep apnea.
Disproportionate Effects on Vulnerable Populations
Climate change disproportionately affects vulnerable populations, making them more susceptible to the adverse health effects of climate change, including sleep apnea. Elderly individuals and children are often more vulnerable due to their reduced physiological resilience to extreme temperatures and other environmental stressors. Low-income communities and those in developing countries often lack access to adequate healthcare and cooling resources, further exacerbating their vulnerability.
Addressing these inequities is essential to ensure equitable health outcomes for all.
Table Comparing Effects of Climate Variables on Sleep Apnea
| Climate Variable | Potential Effect on Sleep Apnea | Severity | Vulnerable Groups |
|---|---|---|---|
| High Temperatures | Increased airway resistance, reduced sleep quality, potential for exacerbation of existing sleep apnea | Moderate | Elderly, children, individuals with pre-existing respiratory conditions |
| High Humidity | Increased airway resistance, reduced sleep quality, potentially affecting the efficiency of breathing muscles | Moderate | Individuals with pre-existing respiratory conditions, those living in humid climates |
| Air Pollution | Irritated airways, reduced respiratory function, potential for sleep disturbances, exacerbating sleep apnea symptoms | High | Individuals with pre-existing respiratory conditions, those living in urban areas with high pollution levels |
Environmental Factors and Sleep Apnea: Climate Change Sleep Apnea
Our changing climate isn’t just impacting our weather patterns; it’s subtly altering our health, and sleep apnea is one area of concern. Understanding the intricate connections between environmental factors and sleep apnea is crucial to developing effective preventative strategies and targeted treatments. From the pollutants in our air to the extreme weather events becoming more frequent, these factors significantly impact our respiratory systems and, consequently, our sleep quality.Environmental factors play a significant role in the prevalence and severity of sleep apnea.
The composition of the air we breathe, the intensity of weather events, and even the subtle changes in atmospheric conditions can trigger or exacerbate sleep apnea symptoms. This means that a deeper understanding of these environmental influences is key to improving both the diagnosis and management of this prevalent condition.
Air Pollution and Sleep Apnea
Air pollution, a ubiquitous problem in many urban areas, is strongly correlated with sleep apnea. Specific pollutants, such as particulate matter, ozone, and nitrogen dioxide, have been linked to respiratory problems, including the exacerbation of sleep apnea. Particulate matter, tiny airborne particles, can trigger inflammation and narrow airways, leading to difficulty breathing and increased sleep apnea symptoms. Studies have shown a direct correlation between increased exposure to these pollutants and a rise in sleep apnea diagnoses.
Climate change is impacting sleep apnea, a condition that’s increasingly prevalent. The rising temperatures and extreme weather events associated with climate change are contributing factors. Interestingly, the recent documentary, the last twins documentary explained , delves into the complex interplay between genetics and environmental influences, which could offer insights into the broader impact of climate change on health issues like sleep apnea.
Understanding these connections is crucial for developing effective strategies to combat sleep apnea in a warming world.
For example, residents in heavily polluted urban centers may experience more frequent and severe sleep apnea episodes compared to those living in cleaner environments.
Extreme Weather Events and Sleep Apnea
Extreme weather events, including heat waves and floods, can significantly impact sleep apnea. Heat waves, by increasing body temperature, can exacerbate existing sleep apnea symptoms. The body’s efforts to regulate temperature can lead to increased breathing difficulties and more frequent apneic episodes. Similarly, floods can introduce pollutants into the air and water, further stressing respiratory systems and potentially worsening sleep apnea.
These events can also disrupt sleep patterns, adding another layer of stress to the already compromised respiratory system.
Atmospheric Pressure and Humidity
Changes in atmospheric pressure and humidity can also affect respiratory function and, consequently, sleep apnea. Fluctuations in pressure can impact lung function, making it harder to breathe, particularly for those with pre-existing respiratory conditions. Similarly, high humidity can increase the concentration of allergens and irritants in the air, which can worsen symptoms of sleep apnea.
Climate change is undeniably impacting our health, and sleep apnea is one concern. The stress and disruption it causes can be directly linked to a wider range of health problems. Interestingly, the fascinating world of animal digestive systems, as explored in the inside cecot photo essay , might offer some unexpected parallels in our understanding of the human body’s response to environmental changes.
Ultimately, though, the connection between the complex workings of our bodies and the consequences of climate change on sleep apnea remains a critical area of study.
Impact of Environmental Pollutants on Sleep Apnea
| Pollutant | Mechanism of Action | Impact on Sleep Apnea |
|---|---|---|
| Particulate Matter | Inflammation, airway narrowing, reduced lung function | Increased severity and frequency of apneic episodes |
| Ozone | Irritates airways, causing inflammation and constriction | Potentially increased severity of sleep apnea, especially in susceptible individuals |
| Nitrogen Dioxide | Irritates and inflames airways, causing oxidative stress | Increased risk of sleep apnea episodes, particularly in individuals with pre-existing respiratory conditions |
Climate Change and Sleep Apnea Risk Factors
Climate change is impacting human health in myriad ways, and sleep apnea is one area of concern. The changing climate brings with it a complex interplay of factors that can exacerbate pre-existing conditions and introduce new risks for developing sleep apnea. Understanding these connections is crucial for developing targeted preventative strategies and improving health outcomes.The link between climate change and sleep apnea risk factors extends beyond just the immediate effects of extreme weather events.
Subtle changes in temperature, humidity, and air quality can influence the body’s physiological processes, impacting sleep and respiratory health. This, in turn, can lead to increased susceptibility to sleep apnea or worsen existing cases. Identifying these factors and their interactions is essential to developing effective preventative measures.
Potential Risk Factors Exacerbated by Climate Change
Several factors linked to climate change can worsen sleep apnea risk. Heat waves, for example, can lead to increased body temperatures, which can strain the cardiovascular system and potentially trigger or worsen sleep apnea episodes. Changes in air quality, often associated with wildfires or increased pollen counts, can irritate the respiratory system, leading to breathing difficulties and exacerbating sleep apnea symptoms.
Furthermore, the rising frequency and intensity of extreme weather events can disrupt sleep patterns and increase stress levels, both of which can contribute to sleep apnea.
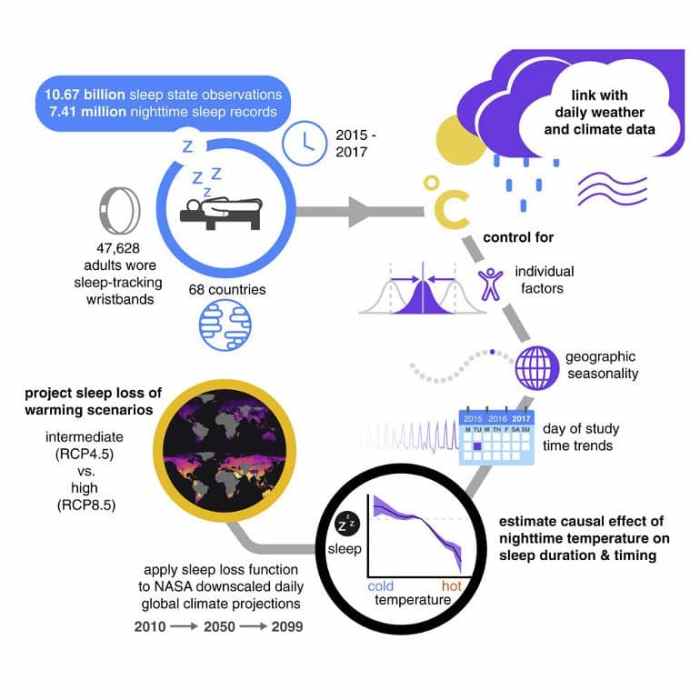
Comparison of Sleep Apnea Prevalence Across Geographical Regions
The prevalence of sleep apnea varies significantly across different geographical regions, often correlating with climate patterns. Regions experiencing hotter and more humid climates, for instance, may have higher rates of sleep apnea, potentially due to the increased strain on the respiratory system under these conditions. Conversely, regions with consistently colder temperatures may have different risk factors affecting sleep apnea prevalence.
Research into the relationship between climate and sleep apnea prevalence is ongoing, but preliminary studies suggest a correlation.
Impact of Climate Change on Pre-existing Sleep Apnea Conditions
Climate change can influence the severity of pre-existing sleep apnea conditions. Increased temperatures can intensify the physiological stress on the body, making it more difficult to maintain adequate breathing during sleep. Furthermore, changes in air quality can exacerbate respiratory problems, leading to more frequent and severe sleep apnea episodes. For example, individuals with pre-existing sleep apnea living in areas experiencing more frequent and intense heat waves might experience a noticeable increase in the severity and frequency of their sleep apnea episodes.
Interaction Between Risk Factors and Climate Change
The following table illustrates the potential interaction between various risk factors and climate change’s impact on sleep apnea.
| Risk Factor | Climate Change Impact | Severity |
|---|---|---|
| Obesity | Increased body mass due to heat stress, poor nutrition | High |
| Air Pollution | Increased respiratory irritation from wildfire smoke and allergens | Medium |
| Heat Stress | Increased body temperature, impacting respiratory function | High |
| Disrupted Sleep Patterns | Extreme weather events, increased stress | Medium |
This table highlights the potential interplay between several factors, suggesting that climate change can amplify the risk and severity of sleep apnea.
Potential Health Impacts of Climate Change-Related Sleep Apnea
Climate change is impacting our sleep, and the resulting sleep apnea can have significant, long-term health consequences. The disruption to our natural sleep cycles, coupled with the increased prevalence of sleep apnea, raises serious concerns about the overall well-being of individuals and communities. Understanding these impacts is crucial for developing preventative strategies and effective healthcare interventions.The amplified effects of climate change, including extreme weather events, air pollution, and heat waves, contribute to a rise in sleep apnea cases.
This escalation, coupled with the existing sleep apnea burden, highlights the urgent need for comprehensive health assessments and proactive strategies to mitigate the long-term health risks.
Climate change is seriously impacting sleep apnea, with rising temperatures and extreme weather events potentially exacerbating existing issues. Interestingly, a recent AI analysis has ranked the top 10 casinos in the world according to various factors the top 10 casinos in the world according to ai , but the connection to sleep apnea, while intriguing, is currently unclear.
Regardless, the link between environmental stressors and sleep health is becoming increasingly apparent.
Long-Term Health Consequences of Sleep Apnea
Sleep apnea, whether exacerbated by climate change or not, carries substantial long-term health risks. It’s not just a nighttime inconvenience; it can lead to significant health problems. Uncontrolled sleep apnea can contribute to a cascade of adverse health outcomes.
Cardiovascular Disease
Sleep apnea significantly increases the risk of cardiovascular diseases. The intermittent pauses in breathing during sleep disrupt the body’s natural rhythms, leading to an increase in blood pressure and stress on the heart. This consistent strain can contribute to the development of hypertension, heart failure, and other cardiovascular conditions. For example, a study in the journal “Sleep Medicine Reviews” highlighted a strong correlation between sleep apnea and an increased risk of cardiovascular events.
Stroke
The impact of sleep apnea on the cardiovascular system is closely linked to an increased risk of stroke. The fluctuations in blood pressure and oxygen levels associated with sleep apnea can damage blood vessels and increase the risk of blood clots, both major contributing factors to stroke. Cases of stroke directly linked to untreated sleep apnea are well documented in medical literature.
Diabetes
Sleep apnea is associated with an increased risk of developing type 2 diabetes. The hormonal imbalances and metabolic disruptions caused by chronic sleep deprivation can impair insulin sensitivity and glucose regulation, potentially leading to the development of diabetes. The connection between sleep apnea and diabetes has been consistently observed in numerous epidemiological studies.
Reduced Cognitive Function
The chronic sleep deprivation caused by sleep apnea can lead to significant cognitive impairment. The brain needs adequate rest to function optimally, and the repeated interruptions in sleep associated with sleep apnea can impair memory, concentration, and overall cognitive performance. This cognitive decline can affect daily life and professional activities.
Mental Health Impacts, Climate change sleep apnea
Sleep apnea is increasingly recognized as a significant factor in the development and exacerbation of mental health conditions. The chronic sleep deprivation and stress associated with sleep apnea can contribute to anxiety, depression, and mood disorders. The link between sleep apnea and mental health is an active area of research, with increasing evidence suggesting a causal relationship.
Correlation Between Sleep Apnea and Health Conditions
| Health Condition | Potential Link to Sleep Apnea | Severity |
|---|---|---|
| Cardiovascular Disease | Increased risk of hypertension, heart failure, arrhythmias | High |
| Stroke | Increased risk of blood clots and vascular damage | High |
| Diabetes | Impaired insulin sensitivity and glucose regulation | Medium to High |
| Cognitive Impairment | Reduced memory, concentration, and executive function | Medium |
| Mental Health Issues | Increased risk of anxiety, depression, and mood disorders | Medium to High |
Adaptation and Mitigation Strategies

Climate change’s escalating impact on sleep apnea necessitates proactive adaptation and mitigation strategies. Addressing this complex issue requires a multi-faceted approach involving individual lifestyle choices, public health interventions, and policy considerations. By implementing these strategies, we can strive to minimize the future burden of sleep apnea in a changing climate.The following sections Artikel preventive measures individuals can take, recommendations for public health interventions, the importance of early detection, strategies for improving sleep hygiene, and a summary of recommendations across different stakeholders.
These strategies are crucial for mitigating the worsening sleep apnea crisis exacerbated by climate change.
Individual Preventive Measures
Individual actions play a pivotal role in reducing sleep apnea risk. Maintaining a healthy weight is a cornerstone of preventive measures. A balanced diet and regular exercise contribute to weight management, thereby reducing the risk factors associated with sleep apnea. Furthermore, avoiding smoking and excessive alcohol consumption are crucial steps to optimize respiratory health. Creating a supportive sleep environment, including a cool, dark, and quiet bedroom, also significantly enhances sleep quality.
- Maintain a healthy weight: Regular exercise and a balanced diet are key components in managing weight. This reduces the strain on the respiratory system, minimizing sleep apnea risk.
- Optimize sleep environment: A conducive sleep environment plays a significant role in improving sleep quality. Maintaining a cool, dark, and quiet bedroom promotes relaxation and enhances sleep. Using earplugs or white noise machines can further aid in creating a conducive sleep environment.
- Avoid smoking and excessive alcohol consumption: Smoking and excessive alcohol consumption can significantly impair respiratory function, increasing the likelihood of sleep apnea. Avoiding these habits can substantially reduce the risk of developing the condition.
- Practice good sleep hygiene: Consistent sleep schedules, avoiding caffeine and alcohol before bed, and engaging in relaxing bedtime routines can improve sleep quality. Establishing a regular sleep-wake cycle can help regulate the body’s natural sleep-wake rhythm.
Public Health Interventions
Public health interventions are essential for addressing the growing prevalence of climate change-related sleep apnea. These interventions should focus on educating the public about the link between climate change and sleep apnea, promoting healthy lifestyles, and supporting accessible healthcare. Investing in community-based programs that offer resources and support for healthy living can create a positive impact on public health outcomes.
Additionally, promoting air quality initiatives can significantly improve respiratory health, reducing the risk of sleep apnea and its related complications.
- Public awareness campaigns: Educating the public about the correlation between climate change and sleep apnea is crucial. These campaigns can highlight the risk factors and encourage proactive measures.
- Community-based programs: Supporting programs that provide resources and guidance on healthy living can empower individuals to adopt preventive measures.
- Air quality initiatives: Implementing strategies to improve air quality can reduce respiratory issues, thus minimizing the risk of sleep apnea.
- Accessible healthcare access: Ensuring that individuals have access to affordable and accessible healthcare services is crucial for early detection and management of sleep apnea.
Early Detection and Management in Vulnerable Populations
Early detection and management of sleep apnea are particularly critical for vulnerable populations. These groups often face socioeconomic and environmental factors that increase their risk. This includes populations residing in regions with high pollution levels, low socioeconomic status, and limited access to healthcare. Implementing targeted screening programs and support systems for these communities can significantly improve health outcomes.
- Targeted screening programs: Developing screening programs specifically for vulnerable populations can ensure early detection and management of sleep apnea.
- Community outreach initiatives: Establishing programs that reach out to vulnerable populations with health information and support can improve health outcomes.
- Addressing socioeconomic disparities: Initiatives that address the socioeconomic factors that contribute to increased risk in vulnerable populations can significantly reduce the burden of sleep apnea.
Improving Sleep Hygiene in a Climate-Altered Environment
Strategies for improving sleep hygiene in a climate-altered environment involve adapting to altered weather patterns. Strategies should incorporate measures that address potential disruptions to sleep patterns due to extreme weather events, such as heat waves or cold snaps. Maintaining a consistent sleep schedule, even during weather disruptions, can help regulate the body’s natural sleep-wake cycle. Using cooling or heating devices to manage indoor temperatures effectively is another critical factor.
- Consistent sleep schedule: Maintaining a consistent sleep schedule, even during extreme weather events, helps regulate the body’s natural sleep-wake cycle.
- Temperature regulation: Using cooling or heating devices to maintain a comfortable indoor temperature during extreme weather events is crucial.
- Addressing light pollution: Limiting exposure to light pollution, especially at night, can promote better sleep quality, particularly in regions experiencing extended daylight hours.
Summary of Recommendations
| Category | Recommendation | Details |
|---|---|---|
| Individual | Maintain a healthy weight | Regular exercise and a balanced diet |
| Individual | Optimize sleep environment | Cool, dark, and quiet bedroom |
| Individual | Avoid smoking and excessive alcohol | Reduces respiratory issues |
| Individual | Practice good sleep hygiene | Consistent sleep schedule, avoiding caffeine/alcohol before bed |
| Healthcare Providers | Implement targeted screening programs | Early detection in vulnerable populations |
| Policymakers | Invest in public awareness campaigns | Educate the public about climate-related sleep apnea |
| Policymakers | Support community-based programs | Promote healthy lifestyles |
Final Wrap-Up
In conclusion, climate change sleep apnea underscores the urgent need for a holistic approach to addressing this emerging health crisis. By understanding the interconnectedness of environmental factors, physiological mechanisms, and risk factors, we can develop more effective strategies for prevention, early detection, and management. This includes individual preventive measures, public health interventions, and proactive healthcare strategies for vulnerable populations.
It’s crucial to prioritize education and awareness, empowering individuals and communities to navigate this evolving health challenge.